Rett syndrome is one of the most common causes of autism spectrum disorder. The causal factor in Rett syndrome (RTT) is a protein called MECP2 (Methyl-CpG-Binding Protein 2) which under normal circumstances acts as a molecular bridge between methylated DNA and the NCoR/SMRT corepressor complex. The recuitment of the NCoR/SMRT complex brings in HDAC3 (Histone Deacetylase 3), which deacteylates histone tails and leads to heterochromatin formation. In patients with RTT, the mutations which predominantly cluster in either the MBD (Methyl-CpG-Binding Domain) or the NID (NCoR/SMRT Interaction Domain) inhibit the interaction of MECP2 with methylated DNA or the NCoR/SMRT complex, respectively.
A study in 2007 showed that reactivation of a silenced endogenous MECP2 in mice led to an almost complete reverstal of the neurological symptoms associated with RTT, providing the first clue that it was a neurodevelopmental rather than a neurodegenerative disease. This prompted the question of whether restoring the function of MECP2 in RTT patients would lead to similar outcomes, meaning that RTT could be treated. If we understood on a structural level how MECP2 interacts with NCoR/SMRT, we could design small drug-like molecules that would possibly restore the binding of MECP2 to its endogenous protein partners, restoring its function. However, while structural data existed about MECP2 bound to methylated DNA, no such data was available about MECP2-NCoR/SMRT complex.
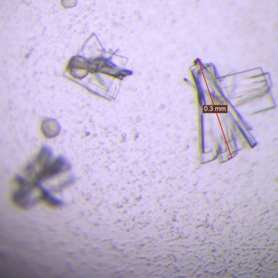
The aim of my PhD project was to solve the crystal structure of MECP2 bound to the main NCoR/SMRT protein called TBL1 (or its paralogue TBLR1), and to understand why RTT mutations lead to a loss of binding to this complex. I crystallised the MECP2 NID peptide in complex with TBLR1 and showed that the most common RTT NID mutations abolish the binding to TBLR1 through either steric clashes, loss of conformational stability, or electrostatic repulsion. I also showed that reciprocal mutations in TBLR1 abolish the binding between it and wild-type MECP2, confirming the importance of the identified residues. Interestingly, several of these TBLR1 reciprocal mutataions are found in the DECIPHER database which map to various intellectual disability disorders. Whether or not they are linked to the loss of MECP2 binding, or whether there are other proteins involved remains unclear.
The other part of the my project was testing the feasibility of developing a plate-based binding assay. This would be used for screening drug precursor libraries to find compounds that could either restore the binding of mutated MECP2 to TBL1/TBLR1 for treatment of RTT, or to abolish the binding of wild-type MECP2 to TBL1/TBLR1 to treat MECP2 duplication syndrome. The latter is a related disorder where the MECP2 gene is duplicated, leading to a similar phenotype as in RTT. I designed a fluorescence-based 96-well plate assay which was successfully used by our collaborators to find compounds that increased the binding affinity of MECP2 to TBLR1. However, the screening was one of the last things I did before I finished my postdoc and moved to Copenhagen to work on microProteins, so I did not have the chance to continue this work.
